Credentialing Explained
Estimated read time: Less than 10 minutes
What is credentialing?
Credentialing is the process of verifying the qualifications and experience of providers. Credentialing is required by payers (aka, insurance companies) to ensure that providers meet the necessary standards to deliver safe and effective care.
Credentialing typically involves:
Verification of Education and Training: Confirming the provider’s education and internship completion, as well as any board certifications.
Licensure Check: Ensuring that the provider holds a valid and current license to practice in their field.
Work History Review: Assessing previous employment and clinical experience.
Background Checks: Looking into any past disciplinary actions, malpractice claims, or criminal history.
Why do I need to be credentialed with Nourish?
Credentialing allows Nourish dietitians to provide in-network, affordable care to patients. Currently, Nourish is in-network with the following insurance companies:
Aetna
Anthem/BCBS
Cigna
United Healthcare
Medicare (must submit the Medicare enrollment application yourself)
Our payers team is actively working to expand coverage! Expect other payers (including Medicaid), to be added in the future.
Luckily, you do not need to wait until you are fully credentialed to see patients! From your very first day, you will be able to see patients as an in-network provider (for any patient with Aetna, Anthem/BCBS, Cigna, or United Healthcare). You will, however, need to complete your credentialing onboarding tasks within your first 45 days, so that our credentialing team can submit your credentialing applications in a timely manner. Failure to complete your credentialing onboarding tasks within your first 45 days may impact patient scheduling.
For Medicare, you will need active credentials before you can see any patients with a Medicare plan. Medicare has unique billing rules, and all providers must have active credentials for any claims to be reviewed. All RDs have to enroll in Medicare on their own if they want to work with this subset of patients.
How long does credentialing take?
Credentialing timelines vary by payer. On average, credentialing applications take 45-90 days to process.
While you will be able to begin seeing patients as an in-network provider before your credentialing has completed, it is expected that you complete the credentialing checklist within your first 45 days (the sooner, the better!)
Our credentialing team works behind the scenes to ensure that your credentialing is completed successfully. If there's anything further they need from you, they'll be in touch!
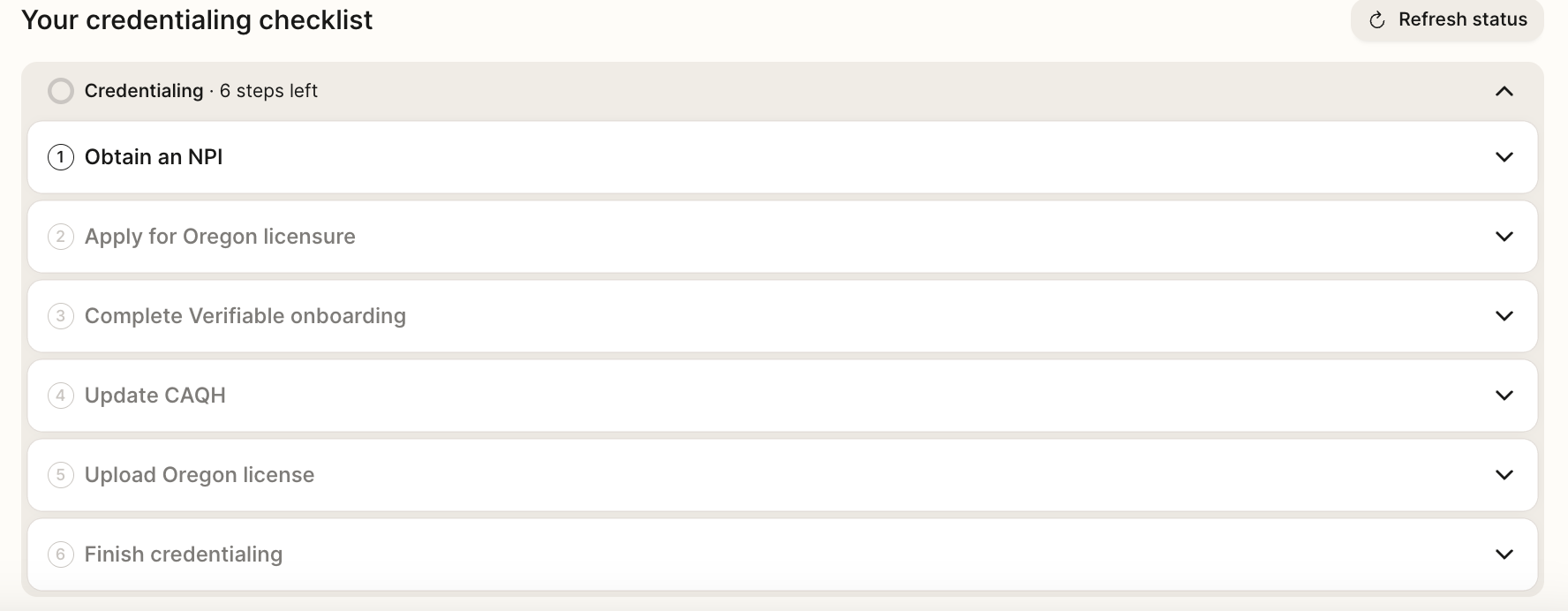
Getting started:
On the Home page of your Provider Portal, you'll find your credentialing checklist, which details all the tasks you need to complete in order to become an in-network provider with Nourish. If you don't see it yet, don't worry! Your credentialing checklist will automatically appear on your first day with Nourish, once your onboarding checklist is completed.
It's important to us that you feel supported throughout this process, so please don't hesitate to reach out to credentialing@usenourish.com, or utilize our New Hire Help Center chatbot, if you require assistance. We're happy to help!